This comprehensive guide explores CAH in women, examining its biological roots, its effects through different life stages, the medical and emotional challenges it creates, and the strategies that enable women to not just manage the condition, but thrive in spite of it.
What Exactly Is CAH?
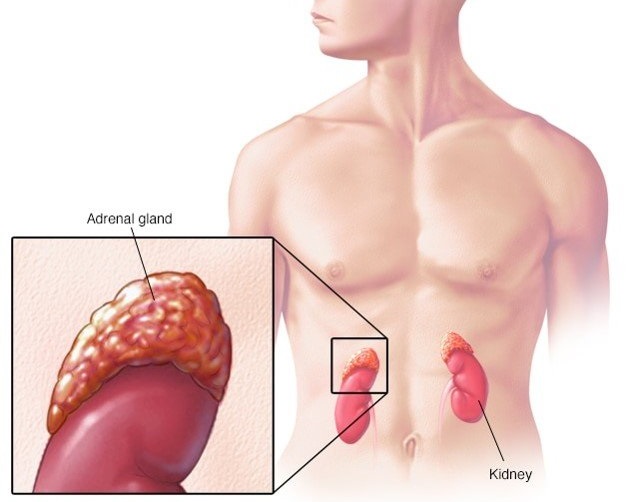
At its core, CAH is a family of inherited disorders caused by mutations in the CYP21A2 gene, which impairs the production of the enzyme 21-hydroxylase. This enzyme is crucial for the synthesis of cortisol (the body’s key stress hormone) and, in many cases, aldosterone (responsible for salt and water regulation). When these hormones are deficient, the adrenal glands compensate by overproducing androgens, or male-associated hormones.
For women, this hormonal imbalance brings profound effects, ranging from differences in genital development at birth to ongoing reproductive and emotional challenges in adulthood.
Two Primary Forms of CAH
-
Classic CAH (severe, early-onset): Typically diagnosed in infancy, it often presents with ambiguous genitalia in girls and can be life-threatening in cases of salt-wasting.
-
Nonclassic CAH (milder, later-onset): Frequently goes undiagnosed until adolescence or adulthood, as its symptoms overlap with more common hormonal disorders like Polycystic Ovary Syndrome (PCOS).
Classic CAH: The Early and Dramatic Form
Women with classic CAH often face health challenges from the very start of life. Newborn screening programs, available in many countries, play a vital role in detecting this form early.
Key Features
-
Ambiguous genitalia in female infants, leading to early investigations.
-
Salt-wasting crisis in some cases, where the body cannot retain sodium—potentially fatal without treatment.
-
Rapid childhood growth that appears promising, but early closure of growth plates often results in shorter adult height.
-
Excess androgen symptoms such as deepened voice, severe acne, and male-pattern hair growth.
-
Menstrual irregularities or absence of menstruation.
-
Reduced fertility, often requiring medical intervention.
Treatment Approach
Classic CAH usually requires:
-
Lifelong glucocorticoid therapy to replace cortisol and suppress androgen overproduction.
-
Mineralocorticoid therapy in salt-wasting cases to stabilize sodium balance.
-
Regular medical monitoring to balance hormone replacement and minimize side effects like weight gain, bone fragility, or growth suppression.
Nonclassic CAH: The Subtle, Often Overlooked Form
Unlike the classic type, nonclassic CAH (NCCAH) may not appear until puberty or later, and it is often mistaken for other endocrine disorders.
Common Symptoms
-
Early or persistent acne.
-
Hirsutism, or unwanted facial and body hair growth.
-
Menstrual irregularities, ranging from unpredictable cycles to infertility.
-
Occasional scalp hair thinning resembling male-pattern baldness.
-
Signs of early puberty such as premature pubic hair development.
Challenges of Diagnosis
Because its features mimic PCOS, many women remain undiagnosed until they experience difficulty conceiving. Testing hormone levels—particularly 17-hydroxyprogesterone—along with genetic testing can confirm the condition.
Treatment Options
-
Some women may not require ongoing therapy.
-
Others benefit from low-dose glucocorticoids to normalize hormone levels, improve menstrual cycles, and enhance fertility.
Why Treatment Matters: The Risks of Ignoring CAH
Untreated or poorly managed CAH can lead to serious complications:
-
Adrenal crisis, a potentially fatal emergency in classic CAH.
-
Severe dehydration and failure to thrive in salt-wasting infants.
-
Metabolic risks, including obesity, insulin resistance, and heart disease.
-
Psychological strain, as visible symptoms like acne or hirsutism can cause low self-esteem, while fertility issues may create emotional distress.
These risks highlight the critical importance of early detection, consistent medical care, and ongoing support.
Reproductive Health and Fertility in Women with CAH
Fertility is one of the most deeply affected areas of a woman’s life with CAH. Elevated androgen levels disrupt ovulation, while hormonal imbalances complicate conception and pregnancy.
-
Classic CAH: Requires close collaboration with endocrinologists and gynecologists during family planning. Pregnancy is possible, but it often demands hormone adjustments and careful monitoring.
-
Nonclassic CAH: With treatment, many women achieve successful pregnancies, though preconception planning is highly recommended.
For those struggling, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) offer viable solutions. Advances in reproductive medicine continue to improve outcomes for women with CAH who want to become mothers.
The Emotional and Psychological Dimensions
CAH is as much an emotional journey as a medical one. Living with symptoms that affect appearance, menstrual cycles, or fertility can challenge a woman’s sense of identity and confidence.
Common Emotional Struggles
-
Anxiety about health and long-term complications.
-
Feelings of being “different,” especially in adolescence.
-
Depression linked to self-image or infertility struggles.
-
Stress over lifelong dependence on medication and medical appointments.
Pathways to Support
-
Counseling and therapy to address self-esteem and anxiety.
-
Support groups that create safe spaces for women to share experiences.
-
Educational resources that empower women to better understand and advocate for their needs.
Emerging Treatments and Modern Care
Medical research is opening new doors for CAH management:
-
Modified-release hydrocortisone designed to mimic natural cortisol rhythms more closely, reducing side effects.
-
Gene therapy, still experimental, but with potential to correct the root genetic mutation in the future.
-
Targeted fertility treatments, improving ovulation and pregnancy outcomes.
-
Integrated care teams, bringing together endocrinologists, gynecologists, dermatologists, and psychologists to deliver holistic support.
These innovations promise more effective and personalized treatment options for women in the years ahead.
Thriving with CAH: Lifestyle and Empowerment Strategies
While CAH cannot be cured, women can take proactive steps to live healthy, fulfilling lives:
-
Adherence to treatment: Staying consistent with prescribed medication and monitoring.
-
Healthy lifestyle habits: Balanced nutrition, regular exercise, and mindful stress management to reduce metabolic risks.
-
Education and advocacy: Learning about CAH helps women make informed health decisions.
-
Community connection: Finding networks of peers who share experiences can provide strength and encouragement.
Empowerment lies in shifting the narrative—from viewing CAH as a limitation to embracing it as a part of one’s resilience journey.
Conclusion: From Survival to Empowerment
Congenital Adrenal Hyperplasia is not just a genetic condition—it is a lifelong story of adaptation, strength, and possibility. For women, the challenges can be immense, touching nearly every stage of life. Yet, with modern medicine, emotional support, and personal empowerment, CAH does not have to define one’s future.
Instead, women can move beyond survival toward thriving—living with confidence, building families, and embracing lives filled with health, connection, and fulfillment.
By reframing CAH not as a barrier but as a journey of empowerment, women can transform struggle into strength, proving that knowledge and resilience remain the most powerful tools of all.
