Pre-Exposure Prophylaxis (PrEP) represents a turning point in HIV prevention — a biomedical innovation that has transformed how we approach controlling the spread of HIV, especially among highly exposed populations. As both a clinician and public health specialist, I have witnessed how PrEP offers not just personal protection, but powerful ripple effects across communities.
This in-depth article explores:
-
The biological and clinical basis for PrEP,
-
Evidence of its effectiveness in trials and everyday healthcare,
-
Real-world outcomes across diverse settings,
-
Challenges hindering broader uptake,
-
And the future of HIV prevention shaped by PrEP.
Let’s explore how PrEP stands as one of the most significant tools in reducing HIV incidence globally.
1. What Is PrEP and How Does It Work?
PrEP, or Pre-Exposure Prophylaxis, involves the use of antiretroviral medications by HIV-negative individuals to prevent infection. It is available in several forms:
-
Daily oral PrEP, commonly using tenofovir disoproxil fumarate (TDF) plus emtricitabine (FTC);
-
On-demand dosing (e.g., 2-1-1 approach) for individuals with intermittent exposure;
-
Long-acting injectable options such as cabotegravir (given every two months) and the newer lenacapavir (given twice yearly).
Mechanism: These medications inhibit reverse transcriptase or disrupt viral capsid assembly, effectively preventing HIV from establishing infection in the body.
2. Clinical and Real-World Effectiveness
2.1 Trial Evidence
-
In the iPrEx trial, daily PrEP reduced HIV acquisition by 44% overall among MSM and transgender women. Participants with drug detected weekly saw up to 99% reduction, and even those using it four times per week achieved 96% prevention efficacy Wikipedia.
-
Across multiple large randomized controlled trials and meta-analyses, consistent use of oral PrEP lowered HIV risk by up to 92%, with adherence playing a critical role NCBIPMC.
-
Among persons who inject drugs, daily PrEP reduced the risk by an estimated 74–84%, depending on adherence CDC.
-
Long-acting injectable PrEP, such as cabotegravir, further reduced HIV risk by 69–90% compared to TDF/FTC NCBI.
-
A groundbreaking six-month injectable vaccine, lenacapavir, demonstrated in the PURPOSE-1 study zero HIV infections among adolescent girls and young women — where background incidence was 2.41 per 100 person-years The LancetReddit.
2.2 Real-World Impact
-
The PrEP Impact Trial in the UK (with over 24,000 participants) showed an 86% reduction in real-world HIV acquisition GOV.UK.
-
In Belgium, real-world PrEP use resulted in an HIV incidence of just 0.21 per 100 person-years, underscoring strong effectiveness outside controlled trials BioMed Central.
-
Urban centers with high PrEP uptake, such as San Francisco and Sydney, experienced dramatic drops in new HIV infections—50% reduction in Sydney over 24 months PMC.
3. The Role in Population-Level Prevention
Beyond individual protection, PrEP contributes to larger public health impact:
-
Clusters of PrEP users generate spillover effects: modeling shows PrEP delivery to MSM indirectly reduces HIV incidence among women by up to fivefold through network effects arXiv.
-
Treatment as prevention (TasP) and PrEP are synergistic: communities implementing both see marked declines in overall transmission rates PMC.
4. Challenges and Limitations
4.1 Adherence and Resistance
-
PrEP’s protective power hinges on consistent use. Inconsistent use dramatically reduces effectiveness—even minimal—placing individuals at risk PMCCDC.
-
In rare cases where HIV infection occurs despite PrEP, drug-resistant strains may emerge, limiting future treatment options Reddithivinfo.nih.gov.
4.2 Risk Compensation and STI Incidence
-
Some users may increase condomless sex or number of sexual partners, a phenomenon known as risk compensation. While evidence on increased sexual risk is mixed, the rise in non-HIV STIs remains a concern PMC+1.
-
A recent network analysis in Ohio highlighted that highly connected PrEP users may contribute to sustaining syphilis transmission in certain communities arXiv.
4.3 Access and Equity Gaps
-
Although global PrEP users increased to ~3.5 million in 2023, this falls far short of the UNAIDS 2025 target of 21.2 million The Lancet.
-
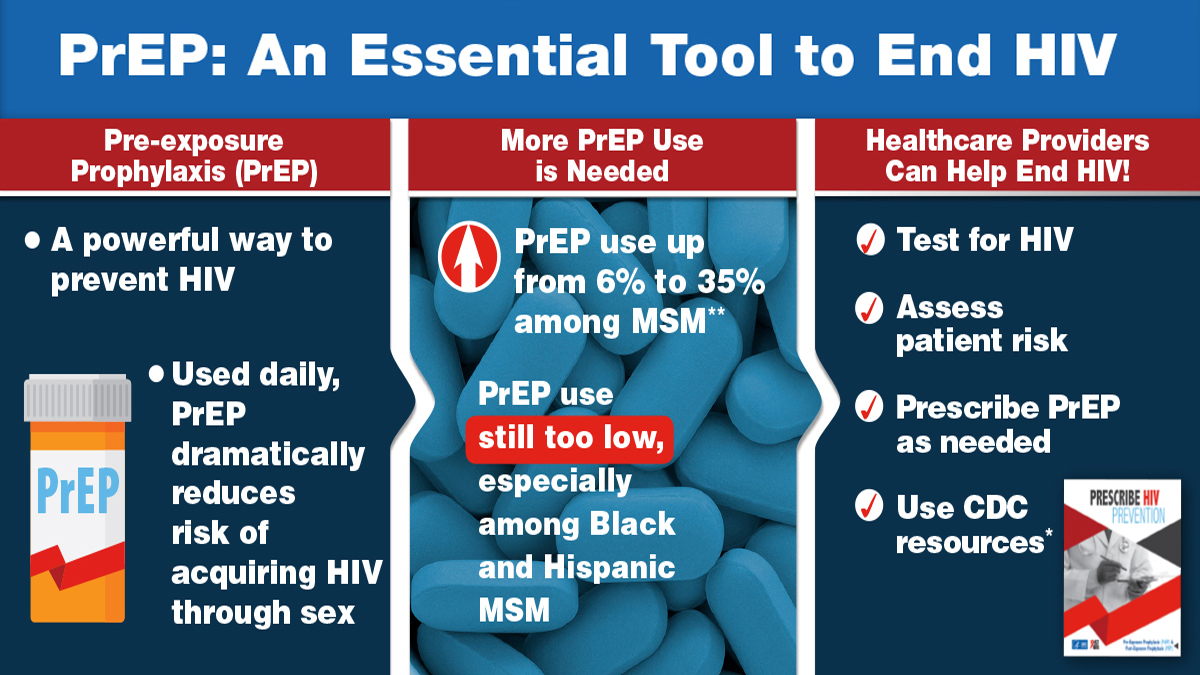
In the U.S., only around 35% of those at risk are prescribed PrEP, with marked disparities: lower uptake among Black and Latino individuals despite higher HIV risk PMC.
-
In Vietnam, engagement of private clinics improved persistence and reduced seroconversion compared to public services, highlighting access challenges and promising strategies to broaden reach PMC.
4.4 Cost and Program Scale
-
In British Columbia, providing PrEP at no cost is projected to reduce new HIV cases by 83% by 2026, accompanied by substantial healthcare savings Wikipedia.
-
Cost-effectiveness modeling in Germany suggests that investing in PrEP may yield €5.1 billion in savings over 40 years Wikipedia.
5. Overcoming the Barriers
To maximize PrEP’s benefit, focused efforts are needed:
-
Enhance adherence support via counseling, reminders, and tailored regimens.
-
Scale up equitable access, especially through programs like Ready, Set, PrEP in the U.S. which offers free medication to those at greatest risk Wikipedia.
-
Integrate PrEP with comprehensive sexual health services, including routine STI screening and reproductive health care NCBIPMC.
-
Deploy long-acting injectables, like lenacapavir, to reduce the burden of daily dosing and elevate effectiveness The LancetReddit.
-
Address stigma and misinformation, ensuring communities know about and trust PrEP, not just MSM or key populations Reddit.
Conclusion
PrEP stands as a cornerstone in modern HIV prevention—highly effective, versatile, and scalable. When used consistently, it drastically reduces individual risk of HIV; when adopted broadly, it transforms communities through reduced transmission and cost savings.
Yet challenges remain: adherence issues, access inequality, rising STI rates, and structural barriers. Overcoming these requires cohesive public health strategies: investing in novel drug delivery, expanding access to underserved communities, integrating with broader health systems, and supporting individuals to remain on PrEP during periods of risk.
As a health professional, I see PrEP’s evolution—from trial to transformative public health tool—as one of our most hopeful chapters in the fight against HIV. With continued commitment, innovation, and equity, PrEP can help us dramatically lower HIV incidence—bringing us closer to ending the epidemic.
